Abstract
Background
IG/TR-based minimal residual disease (MRD) is a faithful marker of response to therapy and the strongest predictor of relapse in acute lymphoblastic leukemia (ALL). In adults with Philadelphia chromosome-positive (Ph+) ALL, MRD is commonly monitored by BCR-ABL1 transcript quantification, although its prognostic significance has not been compared to IG/TR MRD to date. Recently, it has been shown that BCR-ABL1 rearrangement may be found and persist in non-lymphoblastic cells in some patients. In the prospective GRAAPH-2014 trial, using a dual IG/TR and BCR-ABL1 MRD monitoring, we aimed to study the biological and clinical significance of persistent BCR-ABL1 clonal hematopoiesis (CH) in adults with de novo Ph+ ALL.
Patients and Methods
The study comprised 156 adults with de novo Ph+ ALL randomized in the GRAAPH-2014 trial. Bone marrow (BM) and peripheral blood (PB) follow-up (FU) samples were collected after each treatment cycle and before hematopoietic stem cell transplantation (HSCT). MRD monitoring was performed by quantification of both BCR-ABL1 transcripts and IG/TCR clonal rearrangements on all available samples and MRD quantification of genomic BCR-ABL1 breakpoint fusion was also performed for 37 patients. MRD results were considered discordant if more than one log10 difference or positivity/negativity discordance on the same FU sample was evidenced. Cell fractions from 14 peripheral blood mononuclear cells (PBMC) samples (T-cells, B-cells and monocytes) were FACS-sorted and evaluated for BCR-ABL1 expression. Achievement of major molecular response (MMR) defined as <0.1% BCR-ABL1/ABL1 ratio after the 4 treatment cycles (MRD4) was the primary endpoint of the clinical trial.
Results
Quantification of BCR-ABL1 transcripts and IG/TR MRD levels on 876 samples from 156 patients (456 BM and 542 PB) identified 54 out of 142 (38%) evaluable patients with consistently discordant MRD results in at least 3 different timepoints, suggesting the persistence of non-lymphoblastic BCR-ABL1-positive cells in these patients and BCR-ABL1 CH. Possible bias related to variable BCR-ABL1 expression was ruled out by genomic BCR-ABL1 quantification on 263 FU samples (r s=0.89, p<0.0001). Analysis of sorted PBMC fractions from discordant FU samples revealed the expression of BCR-ABL1 in mature B-cells, T-cells and/or monocytes in 11 patients, demonstrating the presence of BCR-ABL1 CH. Baseline characteristics of patients with BCR-ABL1 CH (CH+) showed no difference in terms of age, gender and white blood cell counts, but an enrichment in M-bcr breakpoints as compared to CH- patients (46.3% vs 17.1%, p<0.0001). As expected, the rate of MMR at MRD4 was lower (68% vs 95%, p<0.0001), with a trend for more patients who received alloSCT (38/54 (70%) vs 48/88 (55%), p=0.08).
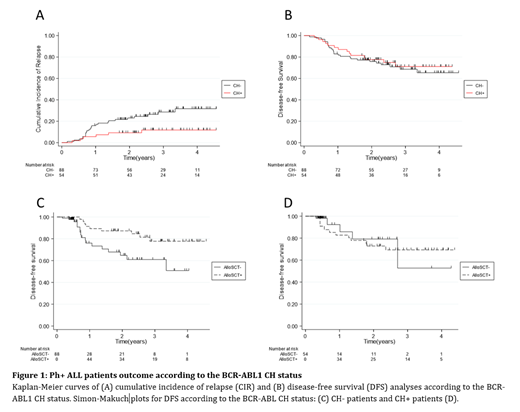
We then evaluated the clinical significance of BCR-ABL1 CH. Unexpectedly, CH+ patients had a significant lower cumulative incidence of relapse (CIR) (panel A, hazard ratio (HR) 0.37, 95% CI [0.15-0.90], p=0.03). However, this lower CIR did not translate into longer disease-free survival (DFS) (panel B, HR=0.85, 95% CI [0.44-1.63], p=0.63). Since an imbalance in alloSCT was observed between CH+ and CH- patients, we tested if the observed difference in CIR may be related to different alloSCT outcomes. When censoring patients at alloSCT, the difference in CIR was indeed no longer significant (subhazard ratio (SHR) 0.48, 95% CI [0.16-1.43], p=0.19). More interestingly, the benefit of alloSCT was restricted to CH- patients. Using alloSCT as a time-dependent variable, DFS was indeed improved by alloSCT in CH- (SHR 0.40, 95% CI [0.17-0.91], p=0.03, panel C) but not in CH+ patients (SHR 1.12, 95%CI [0.32-3.87], p=0.86, panel D) despite a non-significant interaction between CH status and alloSCT.
Conclusion
More than one third of adults with de novo Ph+ ALL displays persistent measurable BCR-ABL1 signal during therapy, likely related to BCR-ABL1 CH. Strikingly, this condition is not associated with a higher risk of relapse nor with poorer overall outcomes in the GRAAPH-2014 trial. Moreover, our results suggest that patients with BCR-ABL1 CH may not be good candidates for alloSCT. By contrast, IG/TR MRD may allow to identify patients with the higher risk of relapse. These results highlight the need for implementation of IG/TR MRD in adult Ph+ ALL to guide therapeutic decisions.
Rousselot: Incyte, Pfizer: Consultancy, Research Funding. Chalandon: Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Amgen: Other: Advisory Board; Incyte: Speakers Bureau; Incyte, BMS, Pfizer, Abbie, MSD, Roche, Novartis, Gilead, Amgen, Jazz, Astra Zenec: Other: Travel EXpenses, Accomodation. Straetmans: Alexion: Membership on an entity's Board of Directors or advisory committees. Huguet: Novartis: Other: Advisor; Jazz Pharmaceuticals: Other: Advisor; Celgene: Other: Advisor; BMS: Other: Advisor; Amgen: Other: Advisor; Pfizer: Other: Advisor. Dombret: Amgen: Honoraria, Research Funding; Incyte: Honoraria, Research Funding; Jazz Pharmaceuticals: Honoraria, Research Funding; Novartis: Research Funding; Pfizer: Honoraria, Research Funding; Servier: Research Funding; Abbvie: Honoraria; BMS-Celgene: Honoraria; Daiichi Sankyo: Honoraria. Boissel: SANOFI: Honoraria; CELGENE: Honoraria; Servier: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding; PFIZER: Consultancy, Honoraria; Bristol-Myers Squibb: Honoraria, Research Funding; Incyte: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; JAZZ Pharma: Honoraria, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal